Vaxelis (DTaP-IPV-Hib-HepB), a Hexavalent Vaccine, is Now Available for VFC
To download a PDF version of this notice, click here!
Vaxelis is now available for providers enrolled in the Vaccines for Children (VFC) program. This advisory includes an overview of important information about Vaxelis.
Vaxelis is a hexavalent combined diphtheria and tetanus toxoids and acellular pertussis (DTaP) adsorbed, inactivated poliovirus (IPV), Haemophilus influenzae type b (Hib, PRP-OMP), and hepatitis B (HepB) (recombinant) vaccine. In 2018, FDA licensed Vaxelis for use in children age 6 weeks through 4 years: it is indicated as a 3-dose series for infants at ages 2, 4, and 6 months. ACIP voted to add Vaxelis to the Vaccines for Children (VFC) Program in 2019. Vaxelis became commercially available in the United States in 2021.
Recommendations For Use
Eligible Groups for Receipt of VFC Supplies of Vaxelis
VFC supplies of Vaxelis may be given to VFC-eligible children from 6 weeks through 4 years of age (prior to the 5th birthday).
Licensed Dosing Schedule
Vaxelis is indicated for active immunization to prevent diphtheria, tetanus, pertussis, poliomyelitis, hepatitis B, and invasive disease due to Haemophilus influenzae type b. Vaxelis is approved for use as a 3-dose series in children from 6 weeks through 4 years of age (prior to the 5th birthday). Vaxelis is indicated for use in infants at ages 2, 4, and 6 months.
Recommended minimum ages for administration of Vaxelis (DTaP-IPV-Hib-HepB) vaccine and intervals between doses — United States, 2020*
|
Age/Interval |
| Minimum age for any dose |
6 weeks |
| Minimum interval between doses 1 and 2 |
4 weeks |
| Minimum age for dose 2 |
10 weeks |
| Minimum interval between doses 2 and 3 |
4 weeks |
| Minimum age for dose 3 |
24 weeks† |
| Maximum age for any dose |
4 years, 364 days (do not administer on or after the fifth birthday) |
† If the third dose of DTaP-IPV-Hib-HepB is given before age 24 weeks, an additional dose of hepatitis B vaccine should be given at
age ≥24 weeks to complete the hepatitis B series.
*DTaP-IPV-Hib-HepB can be used for children aged <5 years requiring a catch-up schedule. However, vaccine doses should not be
administered at intervals less than the minimum intervals indicated in this table.
For guidance on transitioning to Vaxelis and how it fits into the immunization schedule, visit: https://www.vaxelistransition.com.
The Advisory Committee on Immunization Practices (ACIP) recommends that whenever feasible, the same manufacturer’s brand should be used to complete the series. However, if the previous brand is unavailable or unknown, any brand may be used to complete the series. Do not defer immunization solely to wait for a specific brand to be available.
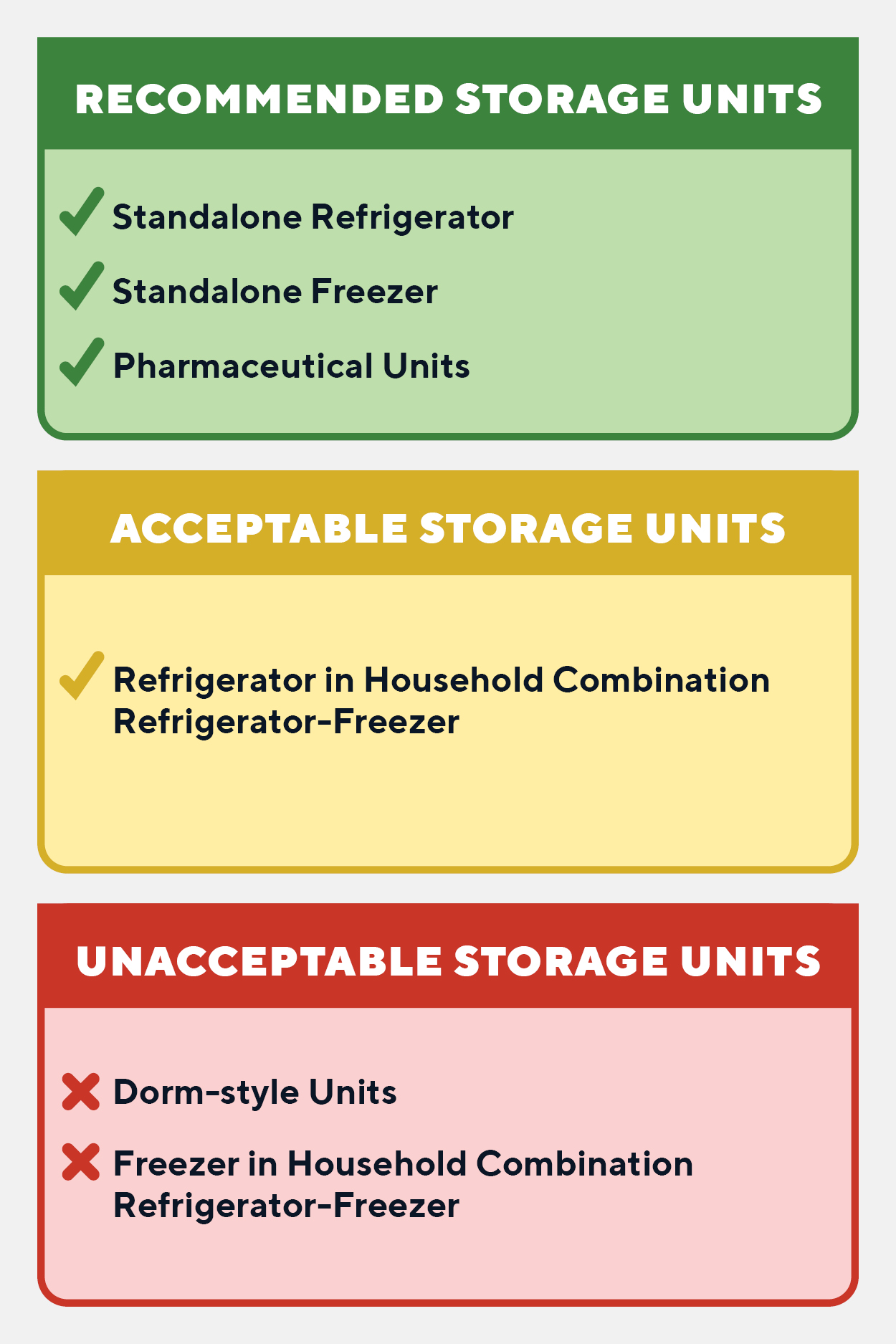
Storage
Vaxelis should be stored at 2º to 8ºC (36º to 46ºF). Do not freeze. Product which has been exposed to freezing should not be used. Do not use after the expiration date shown on the label.
How Vaxelis is supplied
Vaxelis is supplied in a single-dose vial in packages of 10 vials (NDC no. 49281-0590-05). The dosage for Vaxelis is 0.5 mL. Vaxelis does not contain a preservative. The vial stopper, syringe plunger stopper, and syringe tip cap are not made with natural rubber latex.
Administration
Just before use, shake the vial or syringe until a uniform, white, cloudy suspension results.
Inspect the vial or syringe for particulate matter and discoloration prior to administration. If either of these conditions exist, the product should not be administered.
Administer a single 0.5 mL dose of Vaxelis intramuscularly. In infants younger than 1 year, the anterolateral aspect of the thigh is the preferred site of injection. The vaccine should not be injected into the gluteal area.
Vaxelis should not be combined through reconstitution or mixed with any other vaccine. Discard unused portion. Vaxelis is for intramuscular use only.
Precautions and Contraindications
Do not administer Vaxelis to anyone with a history of severe allergic reaction to a previous dose of Vaxelis, any ingredient of Vaxelis, or any other diphtheria toxoid, tetanus toxoid, pertussis containing vaccine, inactivated poliovirus vaccine, hepatitis B vaccine, or Hib vaccine.
Do not administer Vaxelis to anyone with a history of encephalopathy within 7 days of a pertussis containing vaccine with no other identifiable cause.
Do not administer Vaxelis to anyone with a history of progressive neurologic disorder until a treatment regimen has been established and the condition has stabilized.
Ordering and Billing
Vaxelis is available for ordering through the PhilaVax IIS as of today, June 8, 2021. Please contact Jillian Brown (Jillian.Brown@phila.gov) to begin the process of transitioning to Vaxelis at your site. Please note, your practice must choose a single type of combination vaccine to use as part of the primary series. We recommend that sites that are part of a system or are affiliated use the same vaccine presentations across sites to ensure continuity of care and help prevent administration errors.
- CVX code: 146
- CPT code: 90697
Resources
Vaccine Information Statements (VIS):
CDC Morbidity and Mortality Weekly Report (MMWR): https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6905a5-H.pdf.
For guidance on transitioning to Vaxelis and how it fits into the immunization schedule, visit: https://www.vaxelistransition.com.
Product insert for Vaxelis includes additional vaccine information, found at: https://www.merck.com/product/usa/pi_circulars/v/vaxelis/vaxelis_pi.pdf.
Additional information on vaccines and vaccine preventable diseases can be found at: http://www.cdc.gov/vaccines/

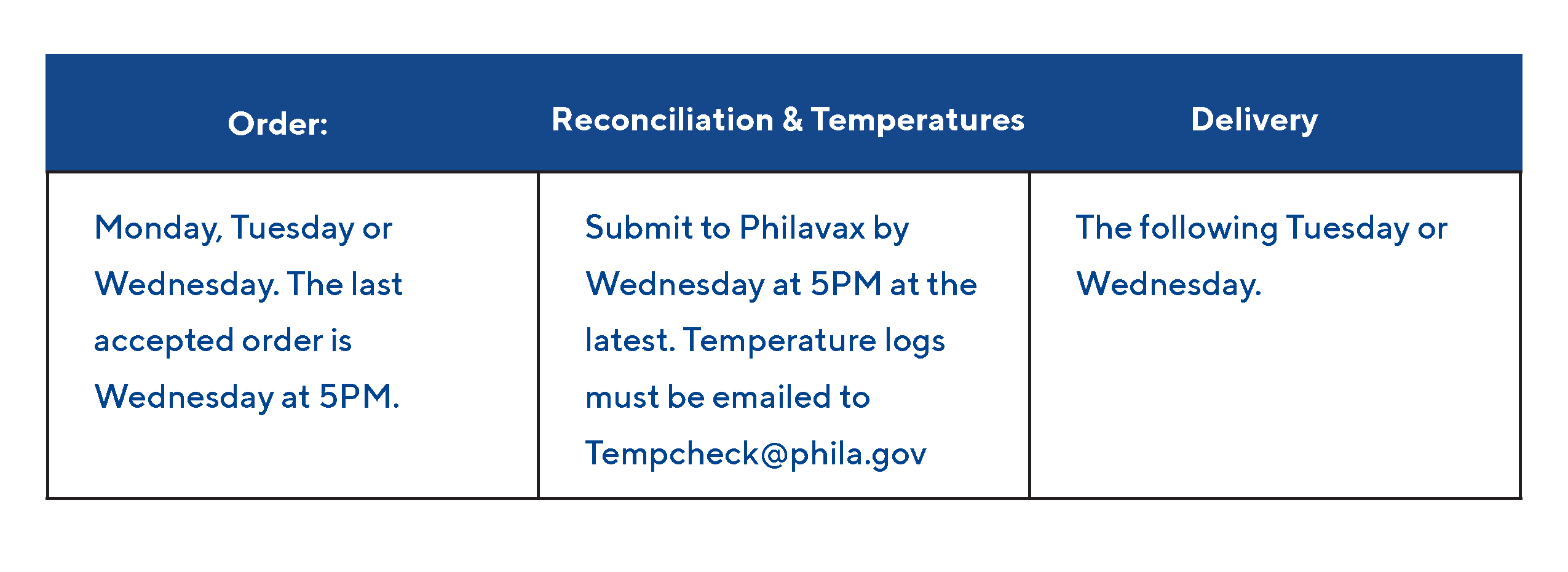 Going forward, the Immunization Program will not process any orders that do not have a closed reconciliation and submitted temperatures by Wednesday at 5PM.
Going forward, the Immunization Program will not process any orders that do not have a closed reconciliation and submitted temperatures by Wednesday at 5PM.